Tag: emergency stroke care
Posted in emergency stroke care
Loved ones may delay emergency care for stroke patients
seek emergency care within the first hour of symptom onset
Posted in emergency stroke care
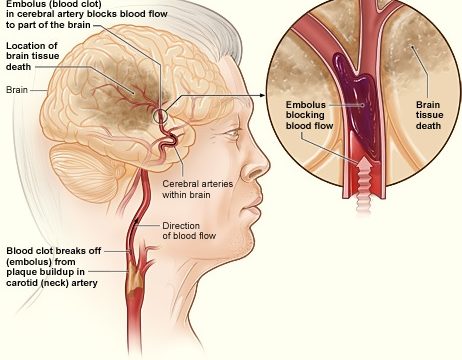
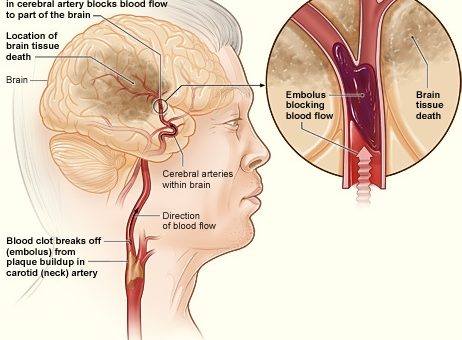
Clot removal effective even six hours after stroke
It is good news; until 2018, we knew that neurosurgeons can salvage living neurons only if they remove the clot within six hours of the block. Now, we know it is not so. They can go ahead with the operation if a patient is ready for the surgery even after…
Posted in emergency stroke care
What is the “golden hour” of a stroke?
Imagine the following trail of events: You start to observe or more F.A.S.T. stroke symptoms and signs in a person; you call an ambulance; emergency responders arrive at the scene; they determine of a stroke; they rush the person to a stroke unit; the person is treated with a blot…
Please be advised that all the information in this resource is for information purposes only and not a substitute for professional medical advice.