Author: Ed Jerard
Help move out of bed after a stroke, but when?
“Help people with acute stroke to sit out of bed, stand, or walk as soon as their doctor says ok”. The above is the latest recommendation from the UK NICE (National Institute for Health and Care Excellence). You can read the exact wording here: But, there is a catch. As…
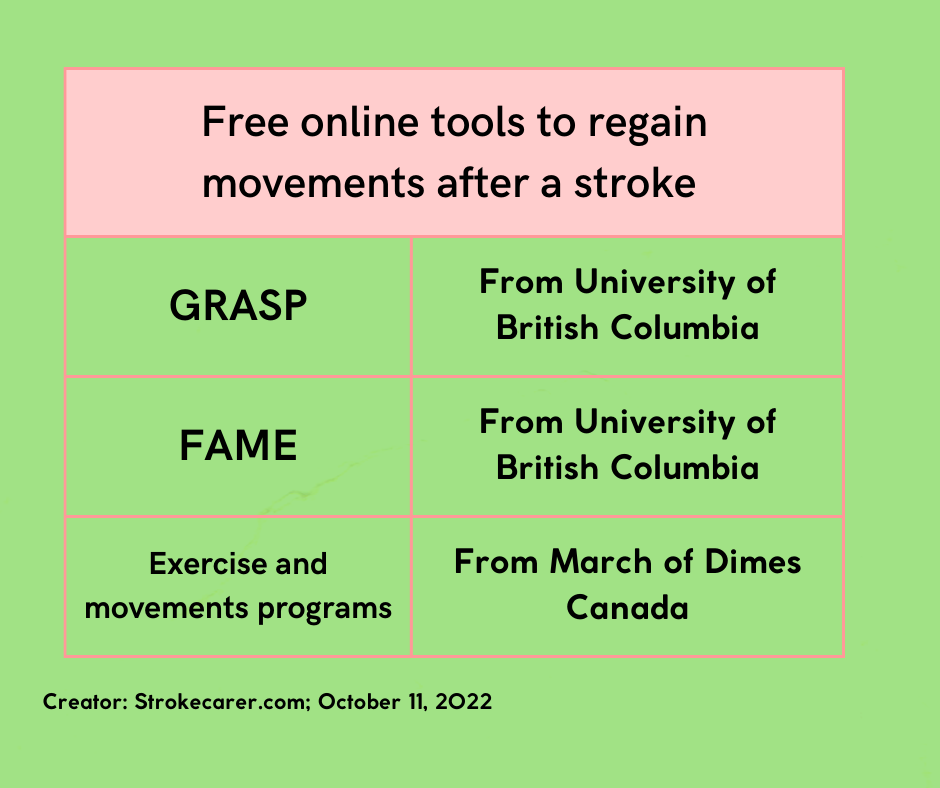
Use free stroke recovery apps to regain movements
This post curates free stroke recovery tools that help to regain movements after a stroke.
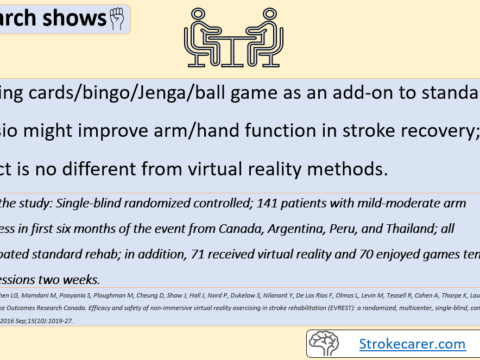
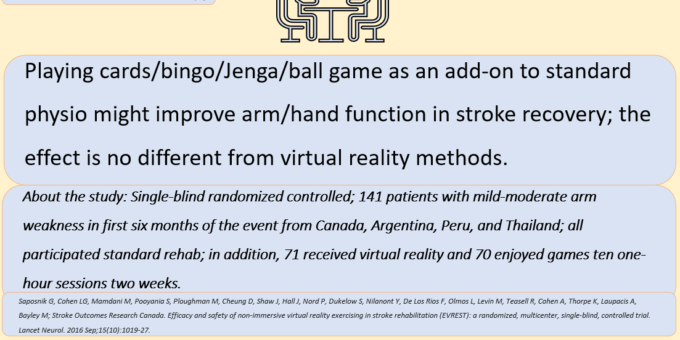
Games like card play help arm/hand stroke recovery
This is great news! Playing cards, dominos, bingo, Jenga, and ball games contribute to arm and hand recovery after a stroke in addition to your standard physio and occupational therapy program. There is another important finding here; its gains are similar to the gains from virtual reality games. In other…
How exercise helps the brain in stroke recovery
Exercise helps the brain to recover lost movements. Find out how.
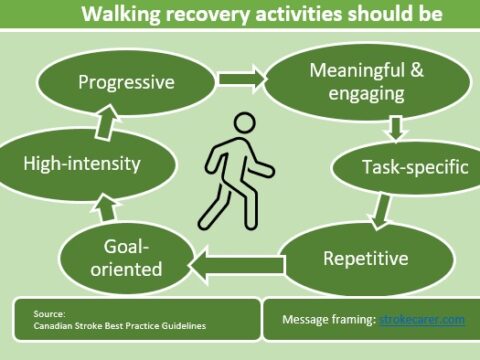
Follow these guides to regain walking after a stroke
Follow these guides to help the brain to recover walking faster and better.
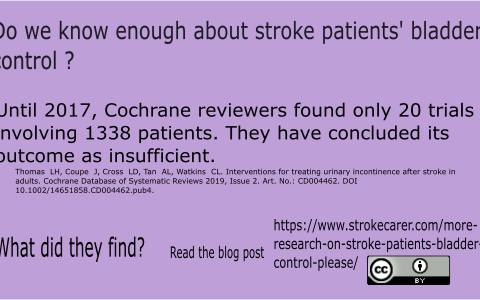
Best practices to regain bladder control
This post deal with how to manage incontinence problems of stroke patients.
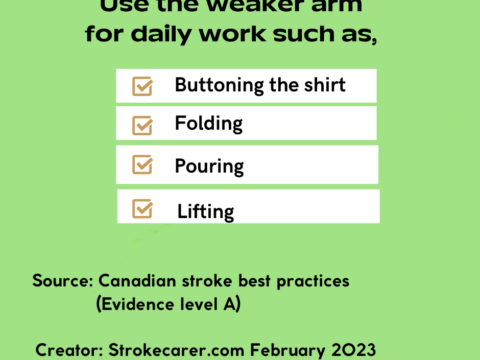
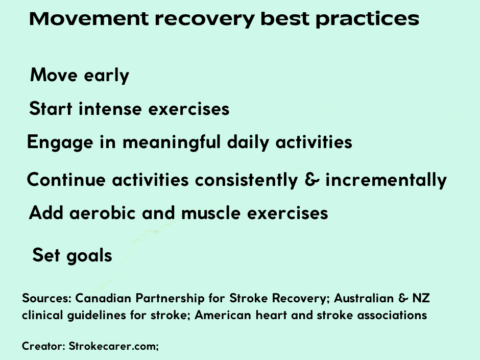
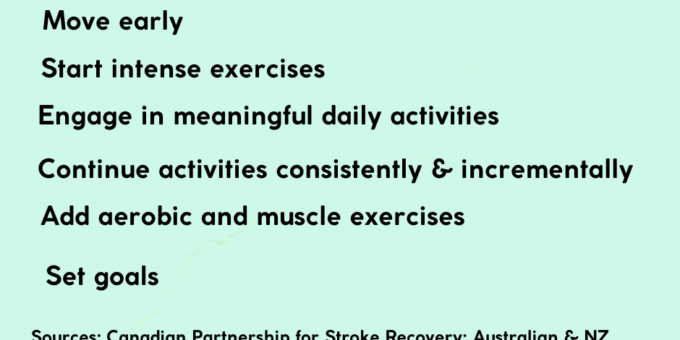
Best practices to regain movements after stroke
Follow these six expert recommended best practices for better, faster recovery after a stroke.
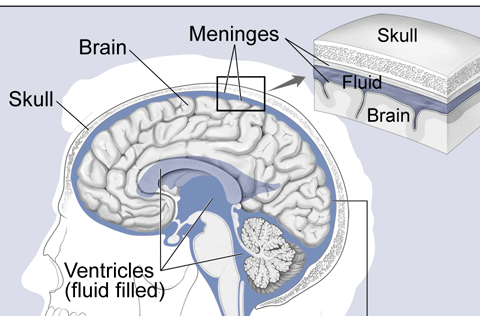
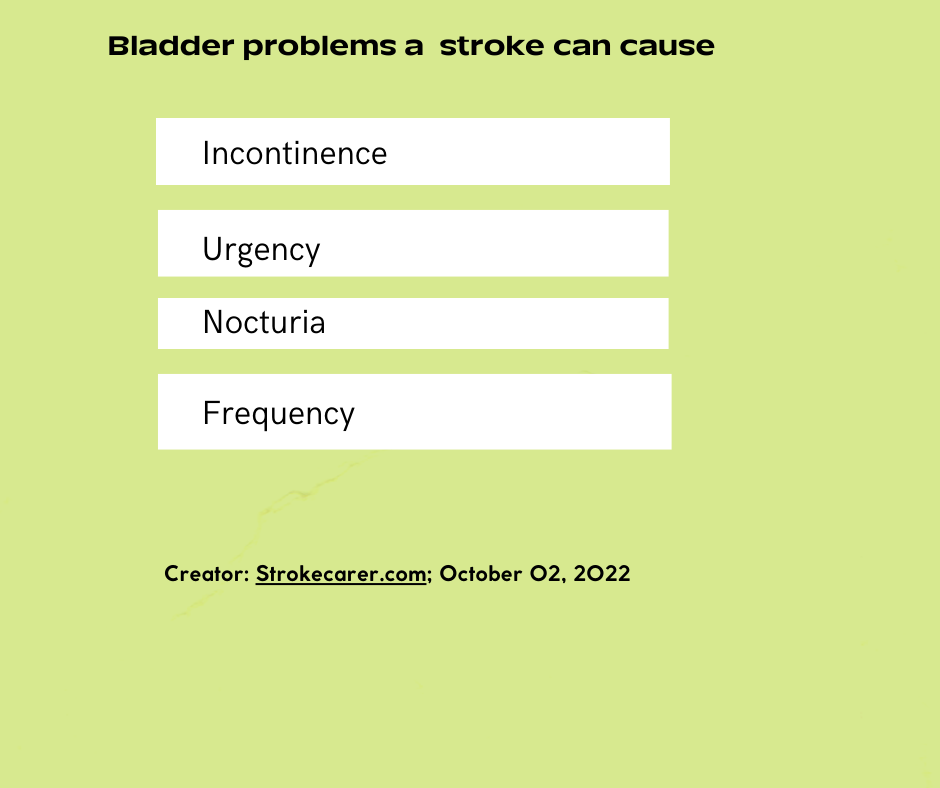
Stroke-related bladder problems
An earlier post explored how stroke can disrupt bladder control. This post looks into stroke-associated bladder problems. These problems could occur due to direct damage to the brain areas that control the bladder and bladder gates. Table of contents Post-stroke bladder problems due to disruption to the brain’s bladder control…
How a stroke causes urine incontinence
Stroke often causes urine incontinence. A good understanding of it help caregivers manage this difficult problem.
Adult diapers, pull-ups, and liners buying guide
Daily, stroke caregivers help stroke survivors wear adult diapers, pull-ups, and liners. They struggle daily if the products do not fit the survivor. We can find a variety of types and brands in the market; you need to spend your precious time and money to search for the most suitable…
Please be advised that all the information in this resource is for information purposes only and not a substitute for professional medical advice.