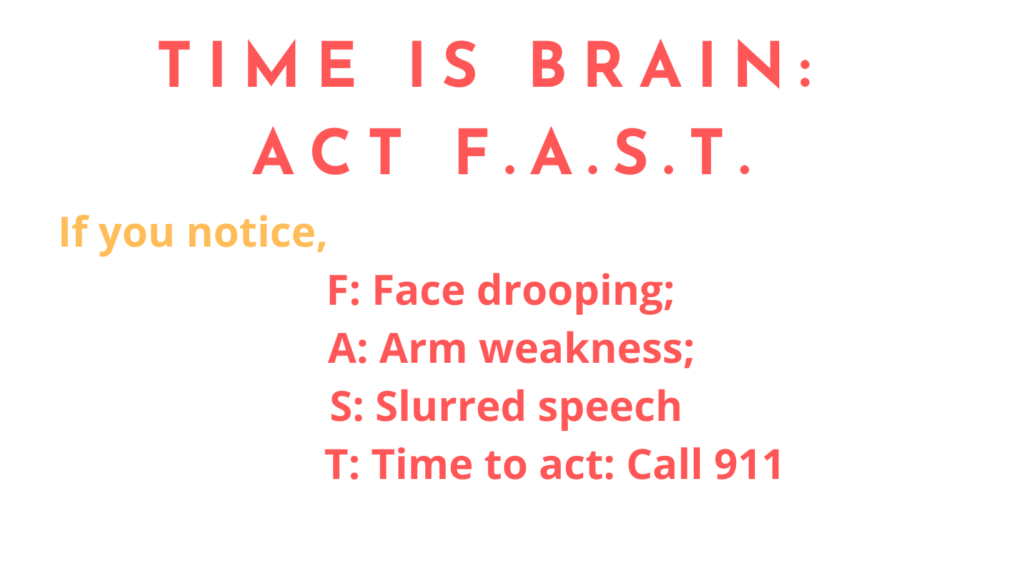
An earlier post explored how stroke can disrupt bladder control. This post looks into stroke-associated bladder problems. These problems could occur due to direct damage to the brain areas that control the bladder and bladder gates.
Table of contents
- Bladder problems due to disruption to the bladder control routes
- Urgency
- Urge incontinence
- Nocturia
- Increased daytime frequency
- Bladder problems due to inability to reach the washroom, a urinal or communicate on time
Post-stroke bladder problems due to disruption to the brain’s bladder control routes
Experts group stroke-associated bladder problems into two;
- Storage problems
- Voiding problems
The storage problems include;
- Urgency,
- Nocturia
- Increased daytime frequency
- Urge incontinence
The voiding problems include;
- Hesitancy
- Decreased stream of dribbling
- Incomplete emptying and hence retention
- Straining
Pain and stress incontinence can also co-exist with the above problems.
Of the two groups, storage problems seem to be the most prevalent and problematic. Nataša Bizovičar‘s 2018 review of published research recognizes frequency, urgency, and urge incontinence as predominant bladder problems. Hence, this post focuses more on this group of problems.
The commonly reported storage problems include;
- The urgency with or without the urge incontinence
- Nocturia,
- Increased daytime frequency,
- Urge incontinence.
The urgency with or without the urge incontinence
What is urge incontinence?
The urgency refers to the sudden, compelling desire to pee which is unable to hold according to the International Continence Society’s glossary.
Research reveals urgency as one of the most common stroke-associated bladder problems. For example, in 2008 a Denmark hospital-based study found that 70 per cent of 482 individuals had urgency a month after the stroke event.
How does the urgency to pee arise?
The normal adult bladder can hold up to about 350 – 450 ml of urine. When the bladder fills, its wall stretches. This wall stretching alerts nerve endings that innervate the bladder wall. The nerve network transmits this message up to the Pontine centre, a place in the lower part of the brain stem (Figure 1). The Pontine center replies. It instructs to contract the bladder wall and open the bladder’s internal gate at the same time. However, the center needs permission from its higher centers which are in the brain’s frontal and other lobes. (Figure 1).
Under normal conditions, the higher centers hold approval until we find a suitable place and time to pee. However, if the higher centers are damaged, either due to a stroke or any other reason, this regulatory mechanism does not happen. This results in a whole range of bladder problems. As a result, depending on the extent of the brain damage, the above problems may manifest even with the filling of small amounts of urine in the bladder.
Urgency severity scale
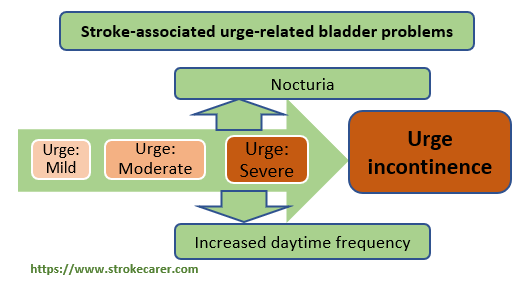
As Figure 2 depicts, researchers view the urgency along a severity scale: Mild, moderate, severe, and urge incontinence. However, urgency is always associated with two problems: Nocturia and increased daytime frequency.
The Urgency Severity scale
Several screening tools exist to recognize and quantify bladder problems. Of those, a group of Korean researchers has suggested the following four-item tool as a simple and practical one. It appears below. They further suggest incorporating it into a bladder diary.
This scale travels from a “no urgency” state to mild urgency, moderate (tolerable) urgency, severe (intolerable) urgency, and ultimately urge incontinence.
| Score | Severity level | Description |
| 0 | no feeling of urgency | I can continue all activities until I reach a toileting facility. |
| 1 | a mild feeling of urgency | I feel the urgency but I can hold it until I reach a toileting facility. |
| 2 | the moderate feeling of urgency | The sensation of urgency causes a compelling desire to void; I need to stop my activity and reach a toileting facility. |
| 3 | the severe feeling of urgency | The sensation of urgency causes a compelling desire to void; I have a difficulty in holding urine. I have to stop my activities to avoid a wetting accident and hurry to the toileting facility. |
| 4 | Unable to hold urine | The urine leaks from my bladder; I have a wetting accident before I reach the toileting facility. |
Urge incontinence
The urge incontinence refers to a situation when the loss of ability to hold until a suitable place and time is met. As mentioned earlier, it could be viewed as the logical result of the urgency spectrum (Figure 1).
Use the following question to determine the presence of urge incontinence.
Is the urge to urinate so strong that urine starts to flow before you reach the toilet or voiding vessel?
Adapted from the DAN-PSS- 1 Questionnaire (Brasso et al. 1994)
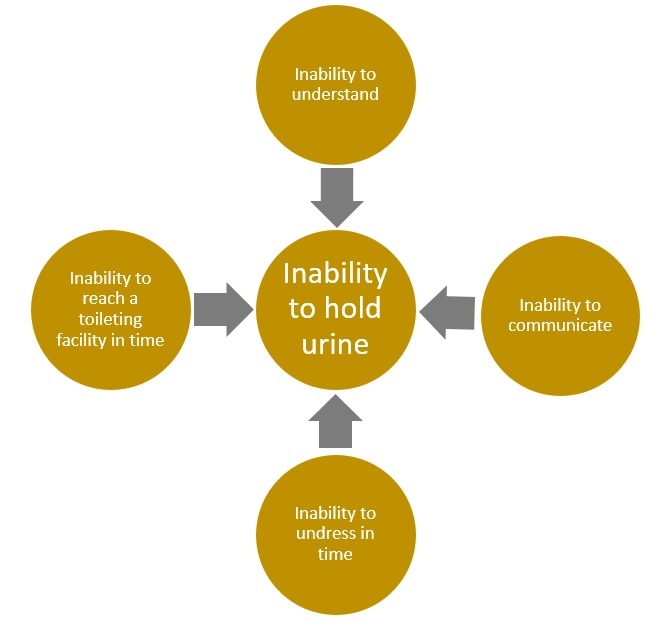
Other forms of incontinence
However, apart from urge incontinence, incontinence with normal bladder function may also occur. Researchers describe incontinence among individuals with normal bladder functions under the following situations;
- When unable to communicate the need to pee
- Difficulty to comprehend the urgency sensation due to cognitive impairment
- When severely restricted to move due to limb paralysis
Moreover, incontinence can also occur due to urine retention resulting in an overflow.
Nocturia
According to the International Continence Society’s glossary, nocturia refers to waking up from sleep at night to pee more than once resulting in disturbed sleep.
Researchers have found nocturia in hospital as well as community settings nocturia as the commonest bladder problem.
Some studies reveal straining and pain as related problems too. They may or may not have incontinence.
Increased daytime frequency
Under normal conditions, an adult fills the bladder and hence feels the urge to pee every 3-4 hours depending on the fluid intake. When someone’s number of times to pee exceeds the above frequency, it could be considered as an increased daytime frequency.
Overactive bladder (syndrome)
All the above-mentioned bladder problems – urgency, urge incontinence, nocturia, and increased daytime frequency – according to the researchers occur due to overactive bladder wall muscle – detrusor. Collectively, researchers bundle these problems under the term, overactive bladder or overactive bladder syndrome.
The International Continence Society defines the overactive bladder as follows;
“Urinary urgency with or without urge incontinence, and with urinary frequency and nocturia, but in the absence of infection or any other disease”.
The core symptom of an overactive bladder is urgency.
Researchers claim only a third of individuals with overactive bladder have urge incontinence. Some may also have an overactive bladder with stress incontinence which arises from a separate mechanism. Stress incontinence arises due to the inability to sustain the extra pressure on the bladder gates. The extra pressure occurs in the form of coughing, sneezing, or laughing.
How to recognize stress incontinence
“Do you experience leakage of urine when physically active(e.g. lifting, sneezing, coughing)?”
Adapted from the DAN-PSS- 1 Questionnaire (Brasso et al. 1994)
Bladder problems due to other stroke-associated impairments
- Peeing problems associated with other impairments that occur due to the stroke
- inability to reach either a toilet or voiding equipment in time
- Speech difficulties
- inability to understand due to a cognitive impairment
- The difficulty of seeing properly