Tag: urine incontinence
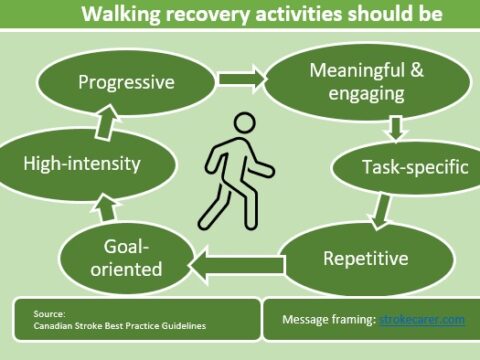
How to deal with incontinence problems of stroke patients
This post deal with how to manage incontinence problems of stroke patients.
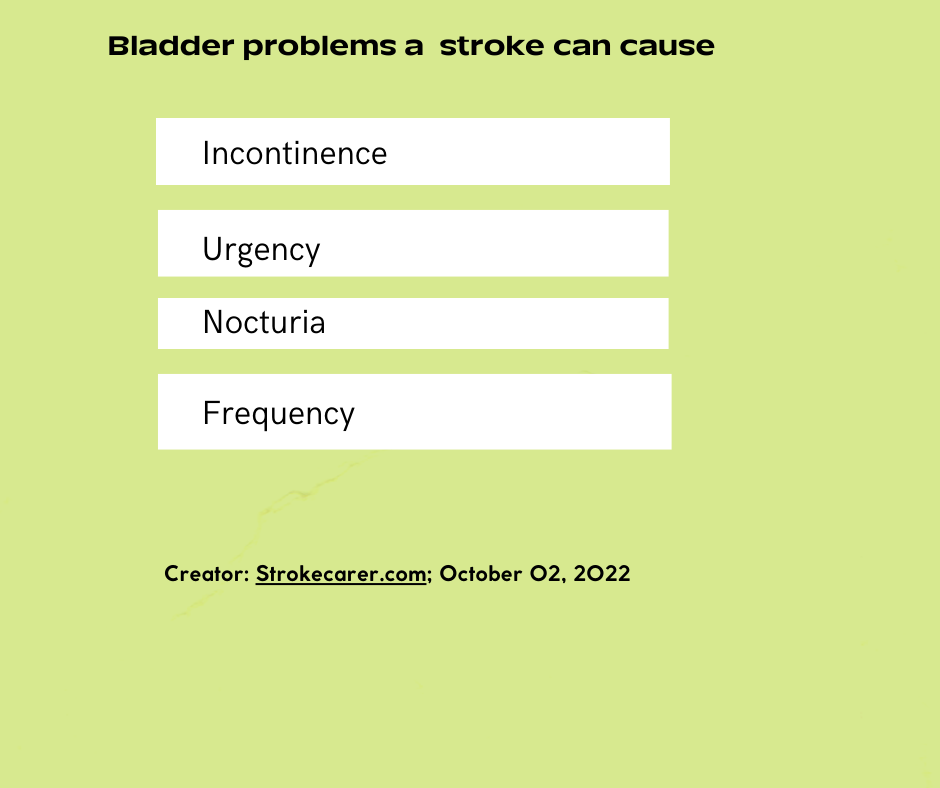
How a stroke causes urine incontinence
Stroke can result in either urinary incontinence or retention. It occurs as a result of the killing of neurons that are responsible in regulating the peeing.
Posted in bladder control
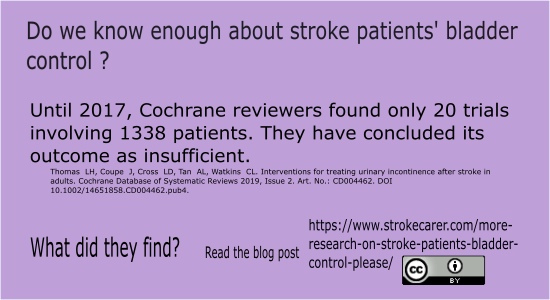
More research on stroke patients’ bladder control needed
Bladder control research among stroke survivors is urgently needed.
Posted in bladder control
Incontinence solutions: The benefits of urine absorbent products
Anatomy of an absorbent products
Cochrane reviews on urine incontinence research
Cochrane reviews about urine incontinence